
The coloured areas represent the white matter hyperintensities in frontotemporal dementia (blue) and Alzheimer’s disease (red). The amount of white matter hyperintensities was associated with the severity of a person’s frontotemporal dementia, including the severity of their symptoms and everyday difficulties, but it was not associated with having vascular risk factors such as high blood pressure and high cholesterol as was expected.

“We also expected to see that people with more severe disease would have more white matter hyperintensities, regardless of disease, but that was only true in people with frontotemporal dementia,” said Dr Landin-Romero, from the School of Psychology in the Faculty of Science. The senior author, Dr Ramón Landin-Romero, from the Brain and Mind Centre said: “We were expecting to see similar amounts of white matter hyperintensities in frontotemporal dementia and Alzheimer’s disease, but we actually found higher levels in people with frontotemporal dementia. The University of Sydney study publishes today in Neurology ®, the medical journal of the American Academy of Neurology. Frontotemporal dementia, which often affects people under the age of 65, mainly results in changes in personality, behavior and problems with language rather than memory.
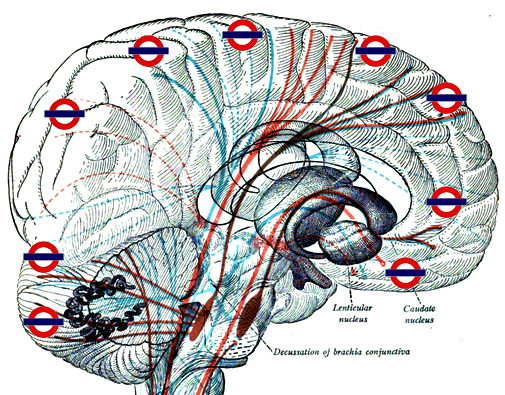
Now a study has shown that white matter hyperintensities are also found in frontotemporal dementia. Areas of brain damage called white matter hyperintensities are commonly linked to vascular/blood vessel-related health problems and have also been linked to Alzheimer’s disease.


 0 kommentar(er)
0 kommentar(er)
